Traumatic brain injuries (TBI) account for thousands of deaths, permanent and temporary disabilities each year.
Not all head injuries are brain injuries. Brain damage caused by a traumatic injury that is confined to one area, is known as a focal injury. Whereas, a widespread TBI is referred to as a diffuse injury.
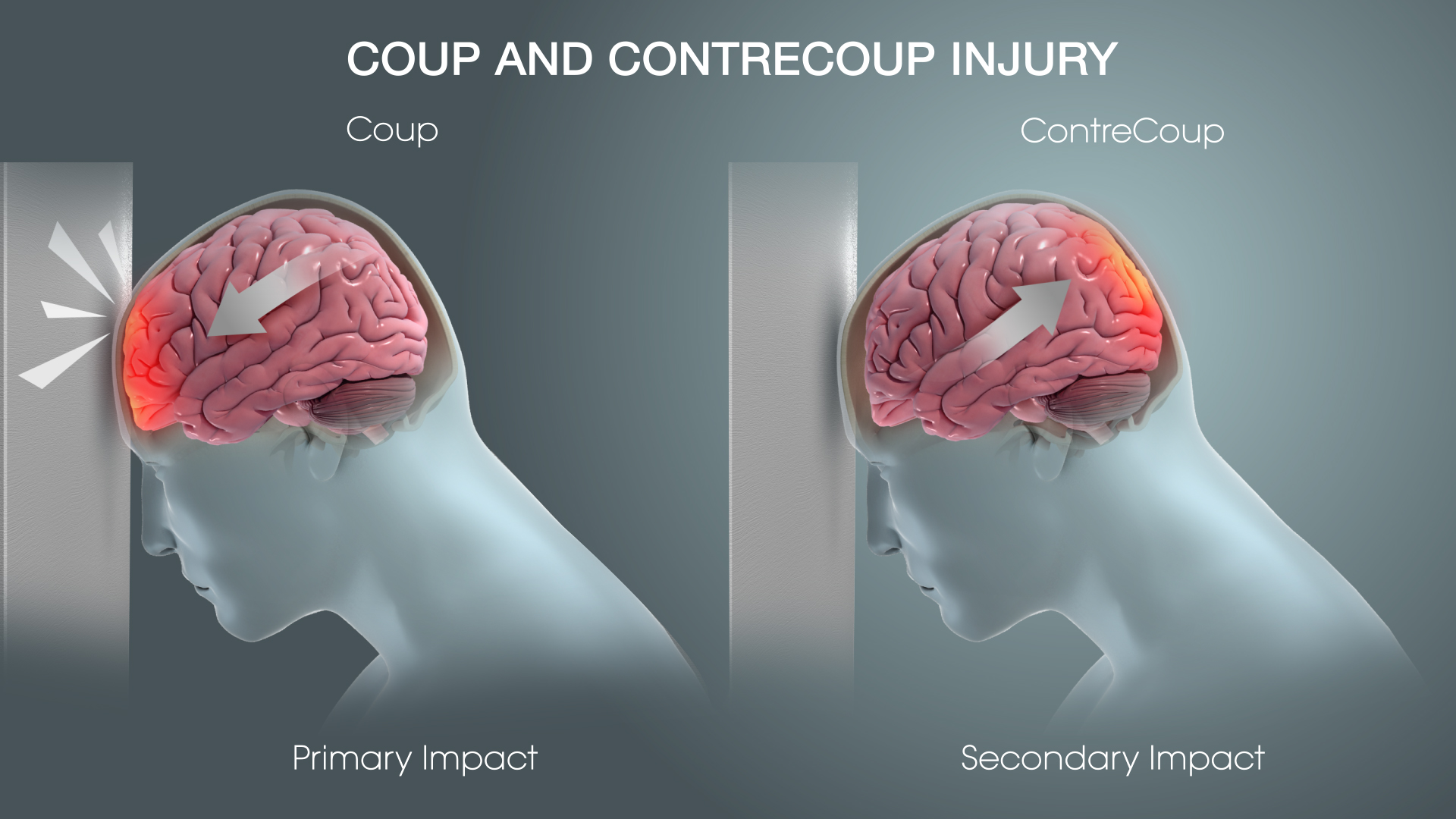
The skull protects the brain from trauma but it cannot absorb the full momentum of an impact. Direct blows may cause skull fractures or even bruise the brain tissue beneath, causing bleeding. The blow can also shift and move the brain inside the skull, hence, the brain injury may not necessarily be located directly below the trauma site.
A brain injury is classified as primary or secondary, based on whether it has an immediate effect on the brain (bleeding and tearing of nerve fibers causing inflammation, metabolic changes) or progresses gradually over a course of time. Secondary brain injuries unfold over time because they are the result of reactive processes that occur after the initial head trauma.
When the blow causes the brain to bounce away and hit the skull directly opposite the trauma site, that is referred to as a contrecoup injury. Such an injury is commonly caused by acceleration/deceleration and rotation forces.
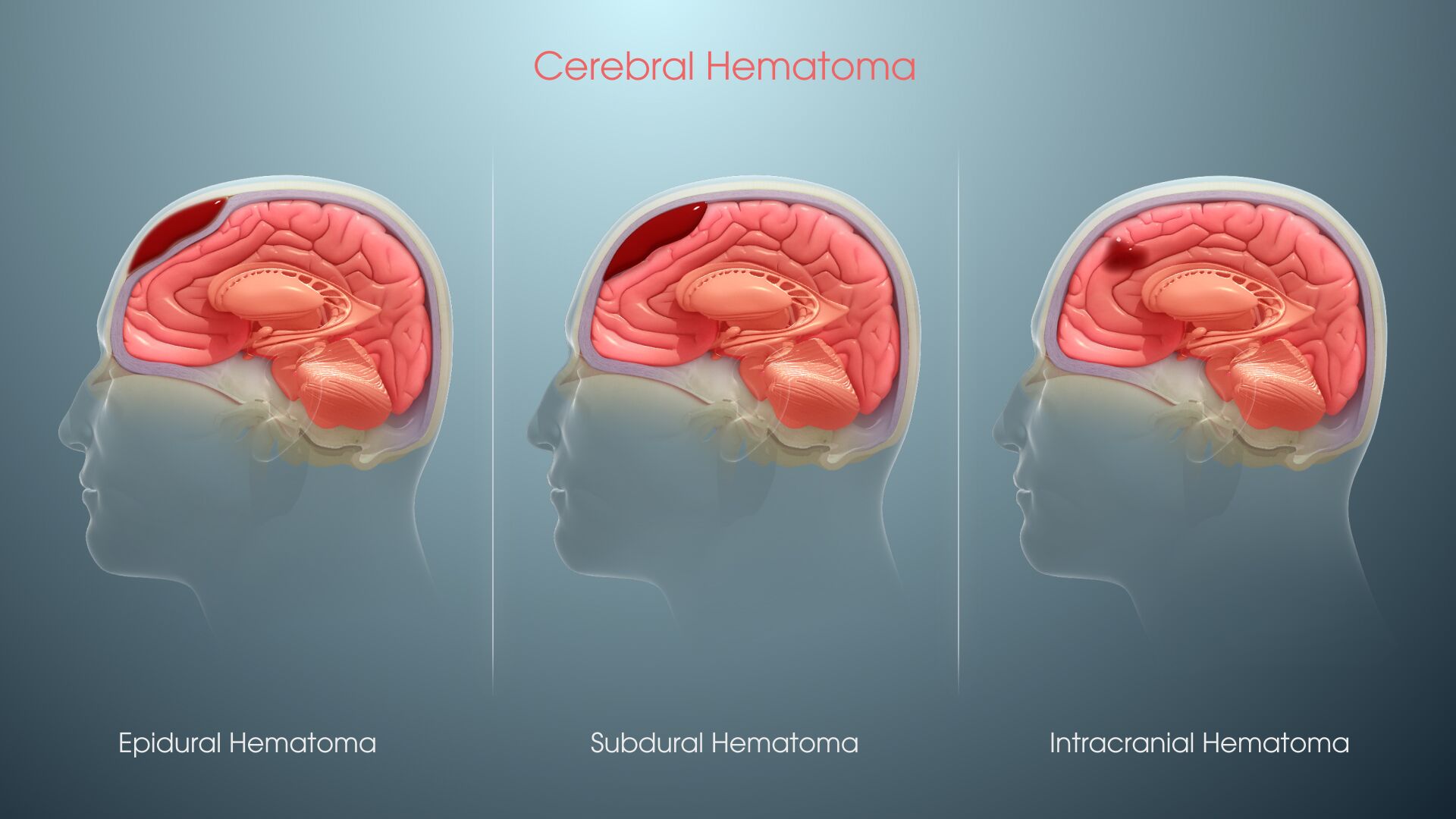
A hematoma occurs when blood pools in brain tissue as a result of damage to major cranial blood vessels. The type of hematoma is defined depending on where the blood collects relative to the meninges, the three protective membranes that surround the brain - dura mater (outermost), arachnoid mater (middle), and pia mater (innermost). They are:
- Epidural – Outside the brain and its fibrous covering, the dura, but under the skull.
- Subdural – Between the brain and its fibrous covering (dura).
- Subarachnoid – Around the surfaces of the brain, between the dura and arachnoid membranes.
- Intracerebral – In the brain tissue.
Hematomas compress the brain and raise the intracranial pressure. They usually need immediate treatment, and can require surgery to drain the blood.
Types of Hematomas
Epidural Hematoma
Most commonly, an epidural hematoma develops with temporal and parietal bone fractures that tear the middle meningeal vessels. Less commonly, they result from tears of diploic veins and dural sinuses.
Epidural hematomas have an overall mortality of 10%. Cranial fractures are present in 70% to 90% of cases. Symptoms of increased intracranial pressure in epidural hematomas with arterial rupture usually develop within hours after the injury. With venous bleeding, they take longer.
There is a natural epidural space around the spinal cord. Spinal epidural hematoma may occur as a result of trauma, but may also develop spontaneously in patients with bleeding disorders.
Subdural Hematoma
Acute subdural hematoma (ASD) can be caused in two ways. The blood that pools up in the subdural space can either come from hemorrhagic contusions and tearing of arachnoid membrane, or from the rupturing of numerous veins that bridge the brain surface and the skull.
The subdural hematoma starts as a flat blood clot between the dura and the arachnoid membrane. Initially, it is not attached to the dura. Fibroblasts, growing from the dura into the clot, organize it. In 5 to 6 days, fibroblast growth causes the blood clot to be loosely attached to the dura. In 10 to 20 days, a loose fibrous membrane is formed between the dura and the clot (outer membrane). Fibrous tissue then grows around the edges of the hematoma and along its inner surface (inner membrane), encapsulating it completely. Maturation of connective tissue results, after several weeks or months, in formation of a sac with a fibrous wall (chronic subdural hematoma). Blood in this sac is absorbed to a variable degree, and the cavity contains clear or hemorrhagic fluid and a loose, vascular connective tissue. Rupture of delicate vessels may cause repeated bleeding in the sac. Fluid may also leak into the cavity from immature capillaries. If a large amount of cerebrospinal fluid enters the subdural space during the traumatic event, it washes off the blood, and no clotting or organization takes place. The histological appearance of the sac is helpful in estimating the duration of the subdural hematoma.
Subdural hematomas generally occur when the head abruptly decelerates, which causes the brain to bounce back and forth within the skull (such as in a high-speed car crash). This type of injury also occurs in shaken baby syndrome, a severe head injury that results when an infant or toddler is shaken forcibly enough to cause the brain to bounce back and forth against the skull.
Subarachnoid Hematoma (SAH)
SAH refers to non-traumatic or spontaneous hemorrhage which usually occurs in the setting of a ruptured cerebral aneurysm or arterio-venous malformation. According to the Brain Aneurysm Foundation, SAH accounts for between 1 in 1250 to 1 in 10,000 visits to the emergency room. Although rare, its symptoms come up quickly post a head trauma. Immediate medical intervention is key to survival.
Intracerebral Hematoma (ICH)
An uncommon yet serious condition, ICH occurs when blood suddenly bursts into brain tissue.
Symptoms like headache, weakness, confusion, and paralysis (particularly on one side of your body), appear suddenly as the buildup of blood puts pressure on the brain and interferes with its oxygen supply. This is a medical emergency requiring immediate treatment.








