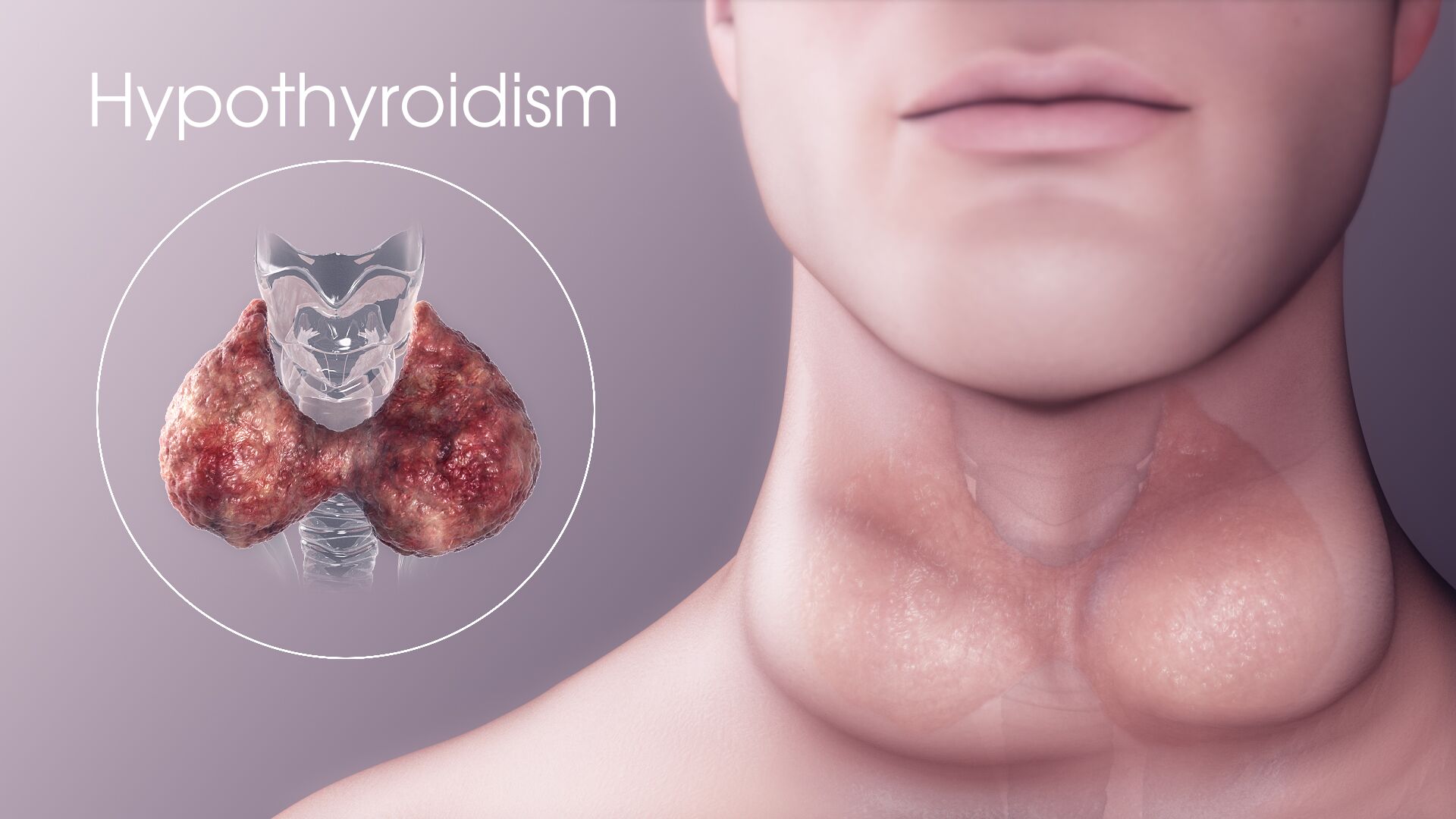
An underactive thyroid gland that does not produce enough thyroid hormone is a medical condition called Hypothyroidism. The thyroid is a small, butterfly-shaped gland situated at the base of neck, and is responsible for synthesizing hormones that regulate metabolism. Lack of thyroid hormone production, hence, causes the body’s functions to slow down.
Causes
- Iodine deficiency is the most common cause of hypothyroidism and goiter worldwide.
- Hashimoto's thyroiditis is a chronic autoimmune condition, in which the person’s immune system attacks their own thyroid gland, causing hypothyroidism. It is more common in women than men and is the leading cause of underactive thyroid in the US.
- Surgical removal of thyroid gland or thyroidectomy in people with thyroid cancer, goiter, thyroid nodules, or Graves' disease also slows or stops the production of thyroid hormones, causing hypothyroidism.
- A few women even develop postpartum thyroiditis for a short period of time. And, some of them may remain permanently hypothyroid.
- Disorders like diabetes mellitus type 1, pernicious anemia, rheumatoid arthritis may also lead to autoimmune thyroiditis.
Pathophysiology
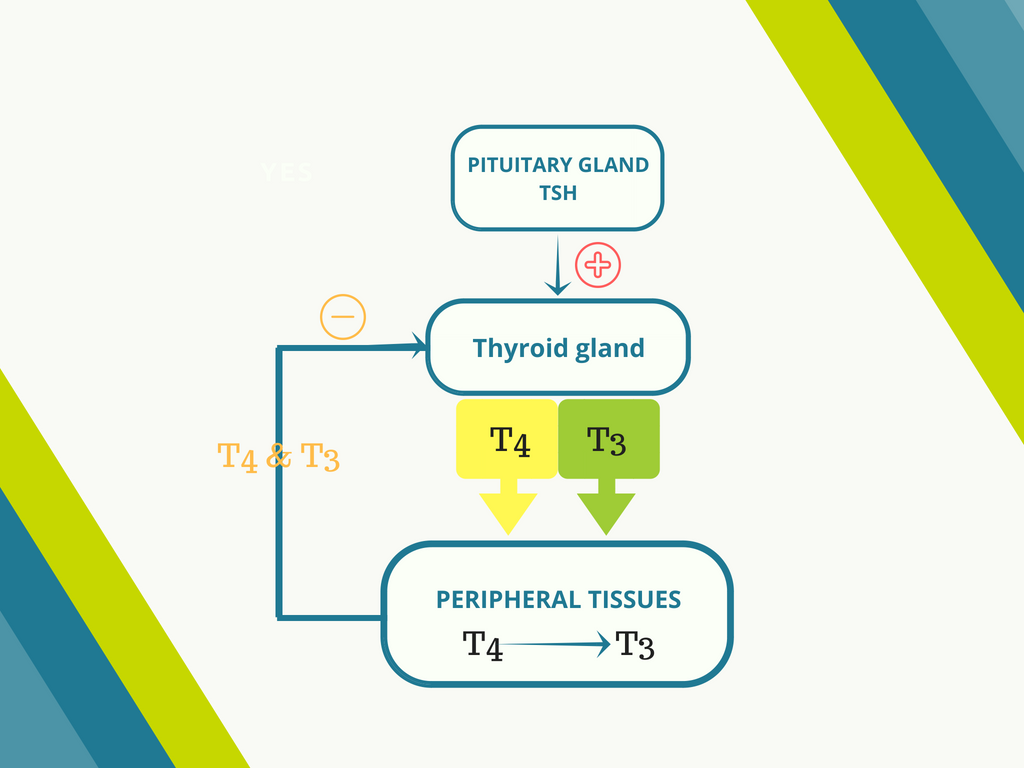
In healthy individuals, under normal circumstances, the thyroid gland secretes a prohormone called thyroxine (T4), which is converted to an active form triiodothyronine (T3) in the peripheral organs. The reaction occurs in the presence of iodothyronine deiodinase. 99.97% of thyroid hormone in the blood is bound to plasma proteins; only the unbound thyroid hormone is biologically active. Overexpression of deiodinase, therefore, leads to hypothyroidism.
Since iodine is vital for the production of thyroid hormone by the thyroid gland and the thyroid stimulating hormone (TSH) secreted by the pituitary controls the entire process, insufficient iodine or TSH can result in decreased production of thyroid hormones.
In pregnant women, the size of the gland increases by 10%, consequently increasing the production of T4 by 50%. This, in turn, increases the iodine requirement too. This may lead to hypothyroidism before or after giving birth.
Management and Treatment
Oral intake of synthetic thyroid hormone
levothyroxine is considered a standard treatment for hypothyroidism. The medication not only restores adequate hormone levels but also helps manage the cholesterol levels that occur as a major symptom of the disease. The dose varies depending on the age, pregnancy status and heart health of the patient.
Mild or subclinical hypothyroidism is suspected when the TSH value drops below 10 mIU/l. Treatment should be considered if a person observes symptoms of hypothyroidism, has detectable antibodies against thyroid peroxidase or a history of heart disease. Unattended subclinical hypothyroidism may increase the risk of coronary artery disease.
Severe hypothyroidism, called
myxedema coma is a crisis condition that requires intensive care. Mechanical ventilation may be required to aid breathing. Fluid replacement and glucocorticosteroid therapy (to compensate for adrenal insufficiency which can occur with hypothyroidism) is also performed. Low sodium levels are often corrected using hypertonic saline or vasopressin receptor antagonists. Intravenous administration of levothyroxine is usually done when the patient is unconscious and needs rapid treatment.