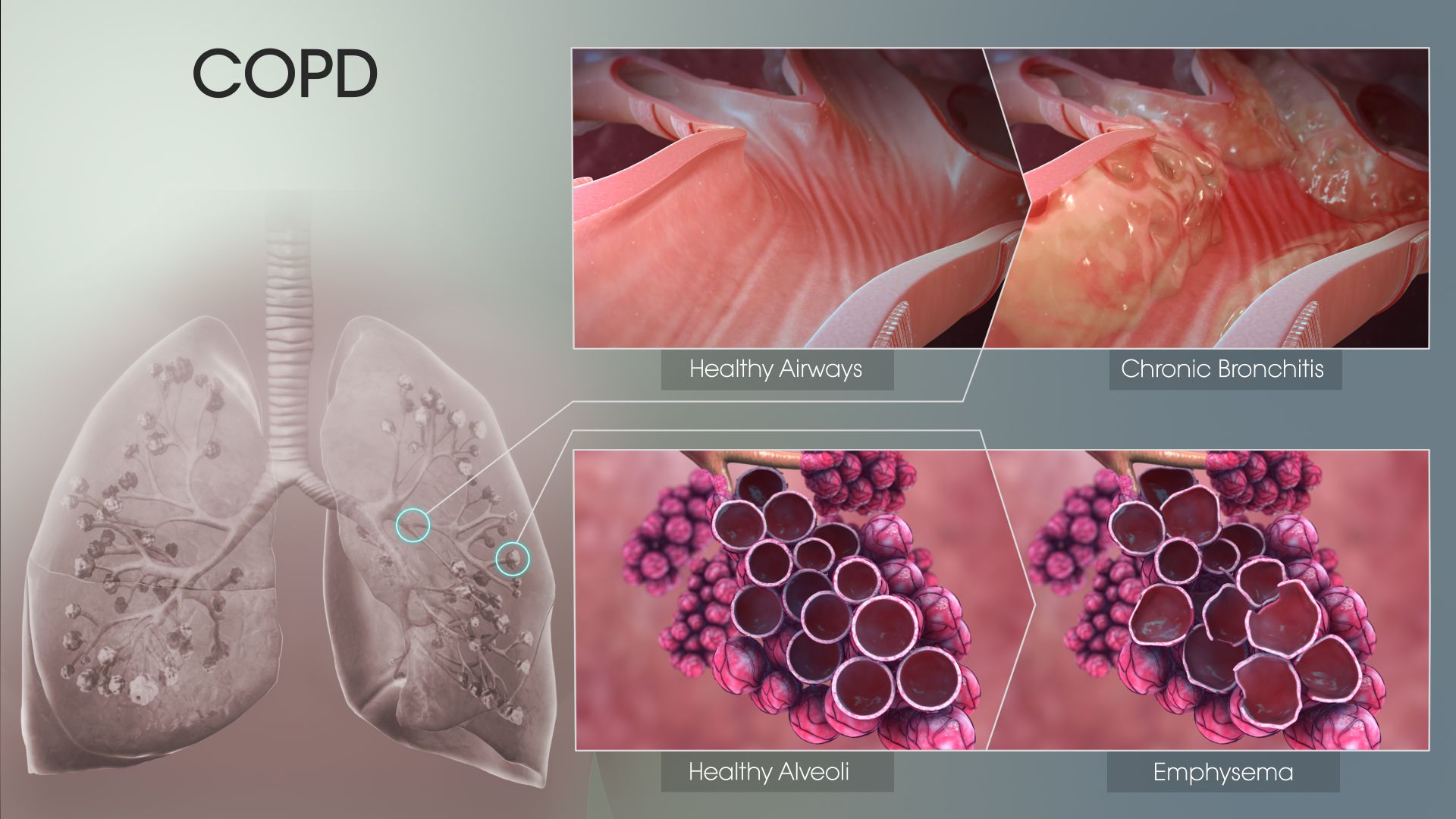
Chronic Obstructive Pulmonary Disease (COPD) is characterized by long-term poor airflow to the lungs. The pathological processes underlying airflow limitation in COPD consist of chronic bronchitis, bronchiolitis, and lung emphysema, although not all patients express all disease entities.
Processes which influence the occurrence of COPD:
- Excessive neutrophil infiltration in the lungs.
- Accumulation of neutrophils leads to high levels of a number of inflammatory modulators, including proteases that have been associated with tissue damage and chemoattractants that recruit additional inflammatory cells.
- Certain components increase the longevity of neutrophils in COPD and substantially add to their accumulation in the lungs.
- In contrast to those of healthy individuals, the neutrophils of COPD patients seem to respond differently to many chemical signals that normally regulate the immune response.
As per the last point, it is clear that the phagocytic capacity of circulating monocytes and macrophages in the alveoli is compromised in COPD, or in other words, neutrophils, ideally designed to fight infection, fail to work in case of COPD.
The identified form of neutrophil behavior is referred to as neutrophil extracellular trap or NET.
Let’s understand NET
Apart from neutrophilic inflammation that predominates in the COPD airways, the progressive clinical course of the disease is punctuated by recurrent destructive reactions which worsen the condition. This is because neutrophil elastase and other neutrophil-derived proteases mediate tissue damage and relentless decline in lung function. Other than the famous cytokines, which are known for modulating the functioning and survival of neutrophils, hypoxia also influences neutrophil function by triggering impaired killing of pathogenic bacteria, enhanced release of proteases, and delayed apoptosis.
Since amount of NET complexes in the lungs of patients is observed to be directly proportional to the severity of their COPD, the biomarker can be exploited to identify the patients who are at a higher risk of disease progression, and also the ones among them who may need special treatments.
Asthma vs COPD
There was a time when distinguishing COPD from asthma in a smoking or ex-smoking patient was a child’s play until studies of asthmatics included measurements of inflammation and studies of patients with COPD included performing methacholine challenges.
| Asthma | COPD |
| Bronchodilator response and airway hyper-responsiveness (AHR) is observed. | No bronchodilator response is observed. In case of smokers, the diffusing capacity of lungs for carbon monoxide is also reduced. |
| Mast cells, lymphocytes and eosinophils are major players. | Neutrophils are mainly involved. Neutrophil activation in the lungs correlates directly with the severity of the symptoms. |
Enter Emphysema…
The main environmental trigger for COPD is smoking, with smokers accounting over 80% of COPD patients. Emphysema is a process of alveolar destruction during which no apparent fibrosis takes place.
Together with bronchiolitis, the above-discussed conditions lead to a reduction of gaseous exchange during respiration. Which factors determine COPD susceptibility is largely unknown and thus there is still much to learn about its etiology and pathophysiology.
Guiding People With Asthma Towards Better Lives
The World Health Organization lists Asthma as the third most life-threatening disease affecting children. Already about 26 million people in the US suffer from asthma, one-third being children. Read More..








