“To resist a compulsion with willpower alone is to hold back an avalanche by melting the snow with a candle. It just keeps coming and coming and coming.”
OCD affects around 3.3 million people in the United States.
As the name goes, Obsessive Compulsive Disorder is most commonly characterised by “obsessions” or recurring uncontrollable, intrusive thoughts and “compulsions” or behaviors that a person feels the urge to repeat over and over; though sometimes it can manifest in different forms as well.
This article is directed towards unraveling the biology of this disorder so that it gets feasible to cure its symptoms, and ultimately, prevent its occurrence.
Psychological, Physiological or Chemical?
While one group of scientists claim it to be a psychological disorder, the other fraction maintains that it stems from physiological abnormalities in the brain. Then there are researchers indicating that OCD may be a result of an imbalance of serotonin (a chemical neurotransmitter believed to be involved in regulating everything from sleep to anxiety) in the brain. However, most of the time OCD cannot be attributed to a single cause and is the result of interplay between several different risk factors.
With so much speculation and uncertainty surrounding this mysterious disorder, we thought of digging up a little science.
Let’s delve into the Human Brain
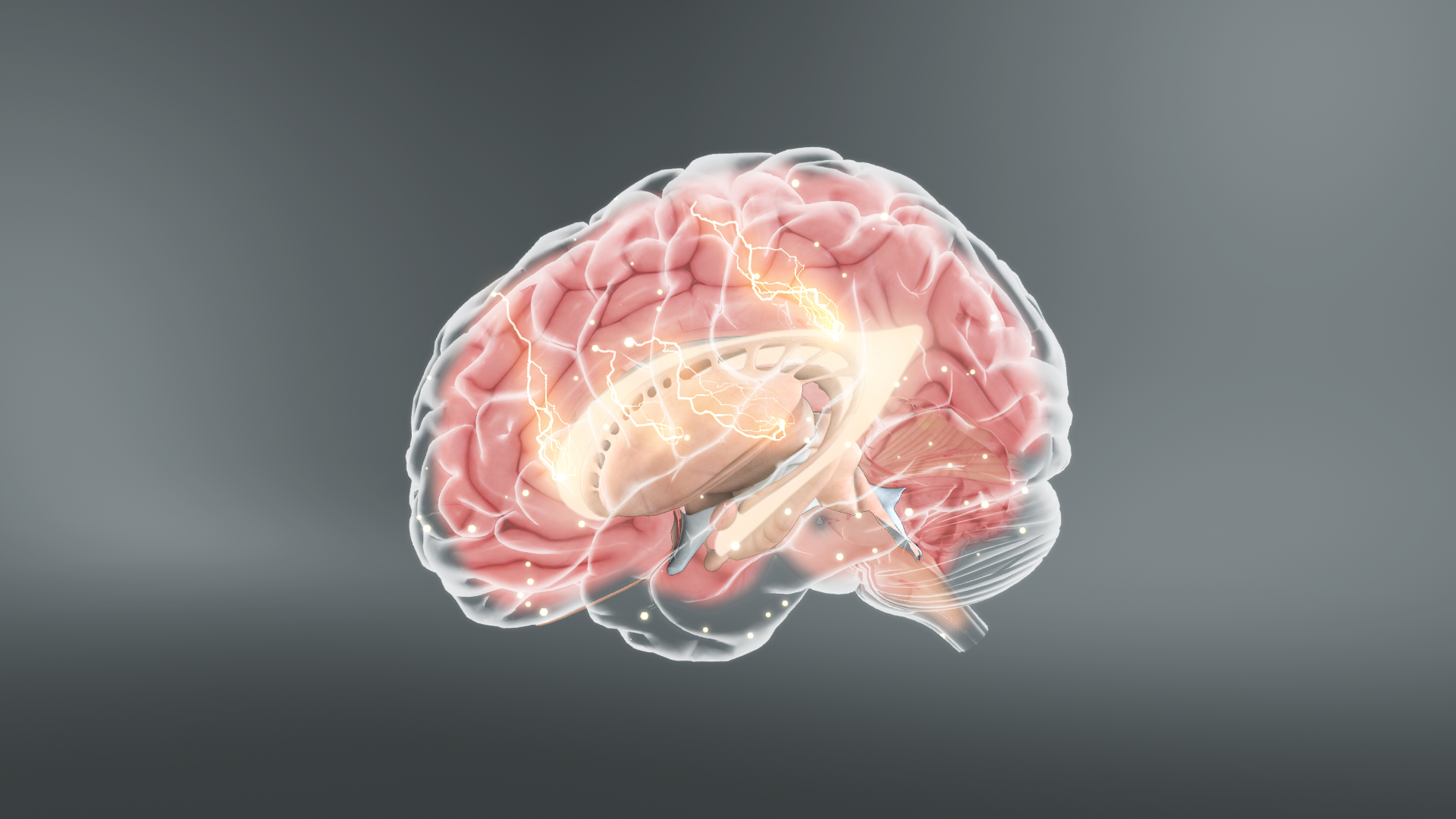
The human brain is comparable to a supercomputer that constantly receives new data in the form of our experiences and keeps decoding it. This is obviously done by different parts that are programmed to handle different aspects of information processing. Consider one area may be responsible to manage incoming sensory data, another might play the role in sorting and prioritize the thoughts, and a third may function to convert those thoughts into emotional responses. They all interact with each other to control the flow of information throughout the brain. A harmonious and synchronized working of these parts together accounts for quick and accurate processing of the information.
Now if the communication system between these parts gets impaired, the information is no more processed correctly and the brain becomes inefficient in governing the body’s response to the thoughts. OCD is one of the outcomes of communication issues between parts of the brain that translate information into thoughts and actions. These parts are the orbitofrontal cortex, caudate nucleus, cingulate gyrus, and the basal ganglia, which when begin to malfunction, inappropriate information is passed through the system and the person becomes overwhelmed by their thoughts and actions.
Brain scans of people with OCD have shown that they have different patterns of brain activity than people without OCD. Different functioning of circuitry within the striatum may cause the disorder. Differences in other parts of the brain and neurotransmitter dysregulation, especially serotonin and dopamine, may also contribute to OCD. Independent studies carried out in OCD patients have consistently found unusual dopamine and serotonin activity in various regions of the brain.
A research at the Wayne State University School of Medicine claims that children with OCD are beset by preoccupations and can't easily move on from certain tasks and behaviors. The notable finding was that the dorsal anterior cingulate cortex, a region of the brain associated with cognitive control, exerts exaggerated brain network effects in OCD.
Understanding OCD
Typically, scientists divide OCD into two areas of study:
- Mechanism, i.e., how the repetition of thoughts occurs, and
- Content of thoughts (ranging from worries about contamination to harming others or self).
After several studies, it has been finally understood that the mechanism of OCD is neurologically mediated and needs to be understood by scientific analysis, while the content of OCD thoughts is best understood via conventional psychoanalysis involving discussions with patients about their backgrounds, fears, and beliefs. Since the biology of OCD remains the same for all patients while the content of OCD thoughts varies considerably among patients, the treatment is focused towards tackling the neurological basis of the disease.
When orbitofrontal cortex and anterior cingulate gyrus get excited, their ability to detect errors is amplified. However, overstimulation of these structures shuns their ability to accurately detect errors and may lead to their firing at inappropriate times. When this happens, OFC and ACG send excessive, erroneous messages to the basal ganglia indicating a non-existent problem. This is exactly what patients report, a sense of "dread and an intractable feeling that something is wrong.”
A prolonged, repetitive state of overstimulation or hyper-excitement of the brain churns out intrusive thoughts, leading to a condition of 'brain lock'. In case of a brain lock, the four areas of the brain namely- orbitofrontal cortex, caudate nucleus, cingulate gyrus, and basal ganglia get locked together and behave as a single entity.
People with OCD exhibit increased grey matter in bilateral lenticular nuclei, extending to the caudate nuclei, and decreased grey matter in bilateral dorsal medial frontal/anterior cingulate gyri, in contrast to the ones with anxiety disorders other than OCD, who evince reduced volumes of grey matter volumes in bilateral lenticular/caudate nuclei as well as in bilateral dorsal medial frontal/anterior cingulate gyri.
A meta-analysis of functional neuroimaging in OCD reported the only consistent findings have been in the orbital gyrus and head of the caudate nucleus.
Lately, a strong evidence has been produced that supports the biological basis for how genes that code for certain receptor proteins might affect obsessive or compulsive behaviors in humans.
The corticostriatal connection is a circuit in the brain of both humans and mice that regulate habitual and repetitive actions. The circuit is made up of certain synaptic receptors. When these receptors were removed or mutated in mice, they exhibited obsessive behavior. The study was published in the journal Cell Reports.
By demonstrating that these receptors have this role in development, researchers down the line will have a target to develop treatments for obsessive-compulsive behavior.
References:
- Voxel-wise meta-analysis of grey matter changes in obsessive–compulsive disorder
- Obsessive-Compulsive Disorder
- Obsessive-compulsive disorder (OCD)
- Understanding Obsessive-Compulsive and Related Disorders
- Study of brain networks shows differences in children with OCD
- OCD-like behavior linked to genetic mutation








