Conventional methods of cancer treatment like chemotherapy, radiation therapy or surgery undoubtedly, have improved patients’ survival. This is true for hormonal therapy also, often used in prostate or breast cancer cases. These conventional treatments, however, offer ‘non-specific’ treatment. In chemotherapy, for example, the cancer therapeutic agents are distributed non-specifically in the body, limiting their ability to target cancer cells while providing excessive toxicity to normal (healthy) cells. This leads to several adverse side effects including hair loss, weakness, and organ dysfunction, and therefore, a low quality of life for cancer patients.
There is a need for devising more efficient therapies. Many new cancer treatments are beginning to cater to this need in oncology, including:
1. Immunotherapy
Cancer’s ability to beat the immune system often complicates treatment. The body fails to recognise cancer cells as threats, and sometimes even promotes their growth. Immunotherapy drugs “mark” cancer cells, making them easier to find. Therefore, the body's defenses can attack tumors more effectively. Immunotherapy is already used to fight some forms of cancer, and many more drugs are in the pipeline.
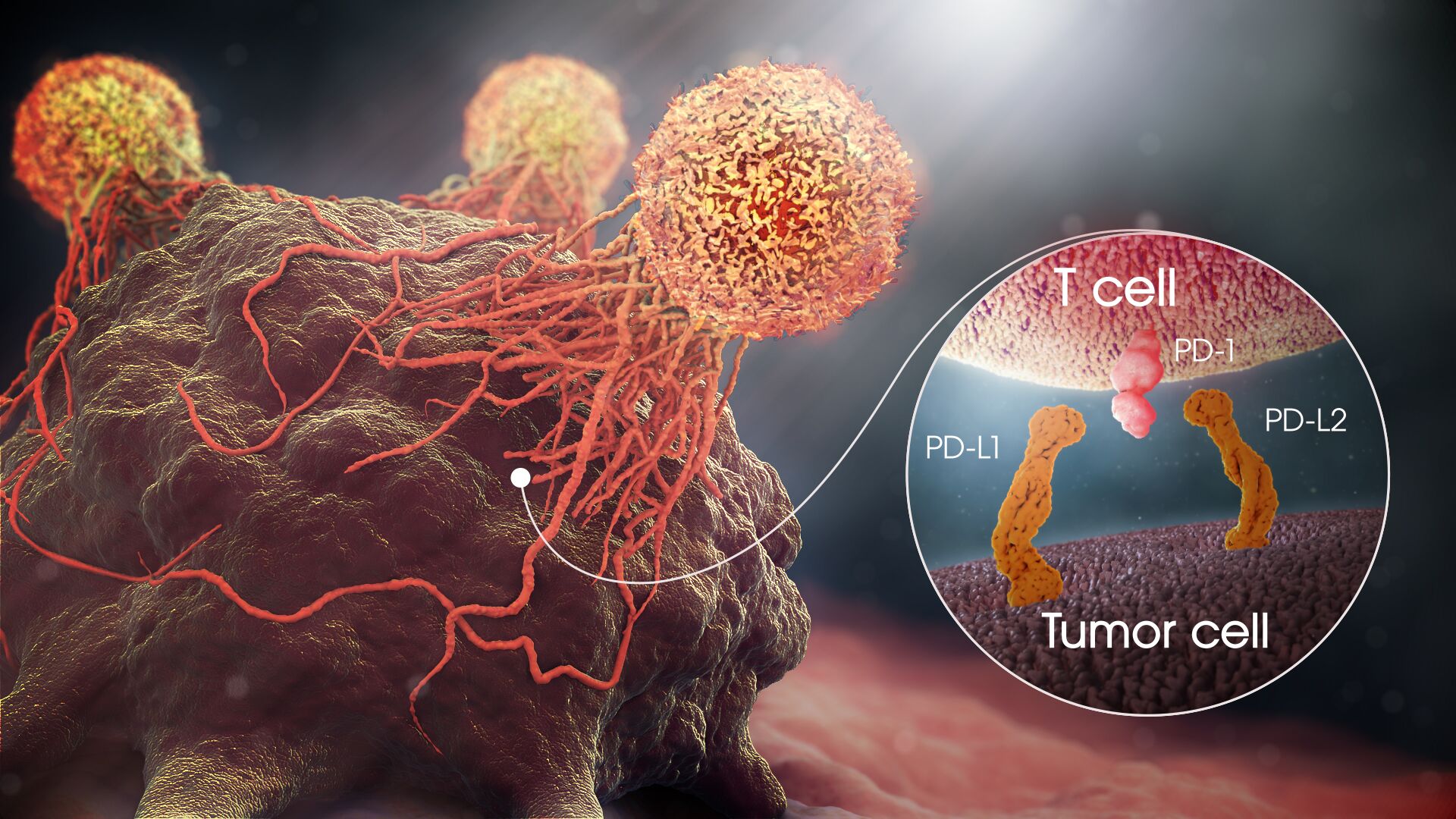
The FDA has approved a form of gene therapy called CAR T-cell therapy. It uses some of the patient’s immune cells (T lymphocytes) and alters them by adding new genes so they can better find and kill cancer cells.
2. Dendritic Vaccine Immunotherapy
Dendritic cells are a part of the body’s normal helper immune system, called the Antigen Presenting Cells, or APCs. They constantly sample the environment in the body looking for invaders, and then present a protein combination to the T- lymphocytes in the lymph nodes. Dendritic cells are, therefore, the alarm; the early warning system.
For decades, cancer researchers have been interested in immunologic treatments against cancer but with little progress. However, recent advances have lead to successful implementation of Dendritic Cell therapy with reports of complete responses even in stage IV cancer patients who have failed all other therapies.
In this treatment, Dendritic cells are harvested from a person’s blood or bone marrow to “arm” them with tumor-specific antigens that guide them to destroy the relevant cancer cells. These cells are then injected back into the body to boost the immune system.
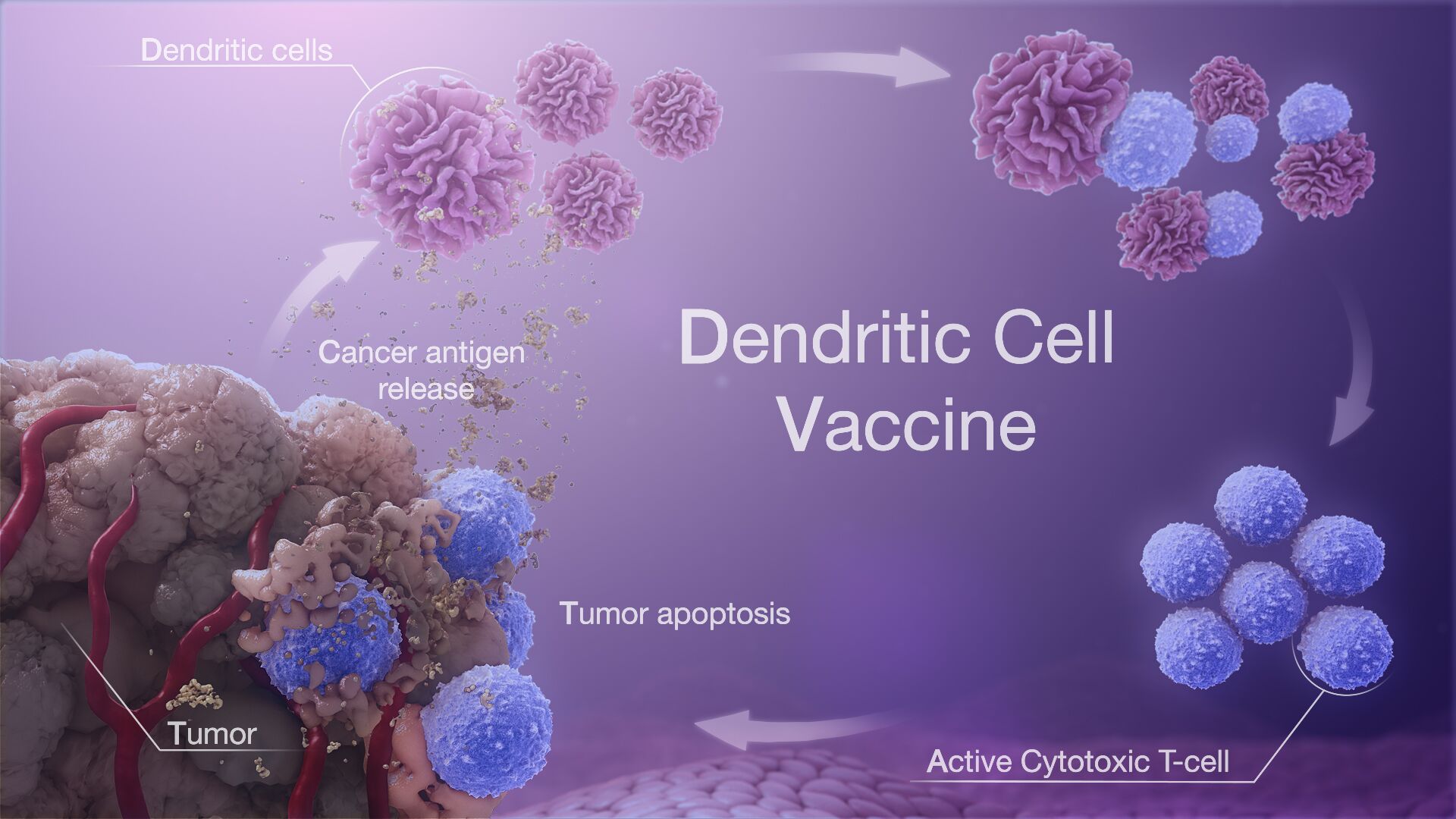
Dendritic Cell Therapy or the so-called Dendritic Cell vaccine is a newly emerging and potent form of immunotherapy used to treat cancer.
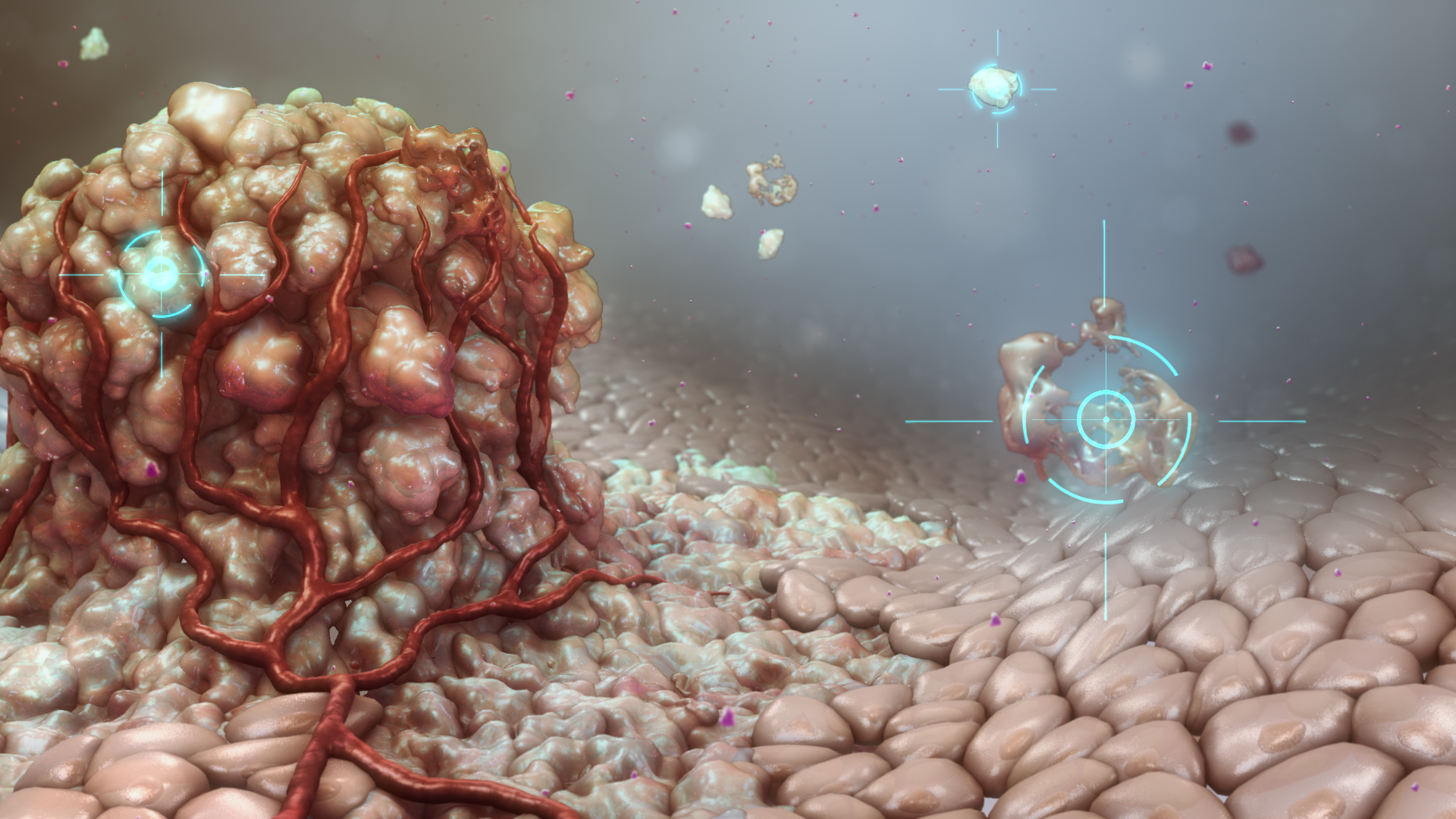
3. The Nanoparticle Revolution
Nanoparticles have garnered much attention in clinical research because they present an opportunity to develop precise, less invasive methods of tackling tumors. They can target cancer cells without harming healthy cells in the surrounding environment, and hence, are considered a vital therapy.
Some nanoparticles have now been created to provide very focused hyperthermic treatment, which is a type of therapy that uses hot temperatures to shrink cancerous tumors. The temperature-sensitive system can carry and release drugs with changes in temperature locally in the tumor region provided by sources such as magnetic fields, ultrasound waves, and so on so that combined therapy such as chemotherapy and hyperthermia can be applied.
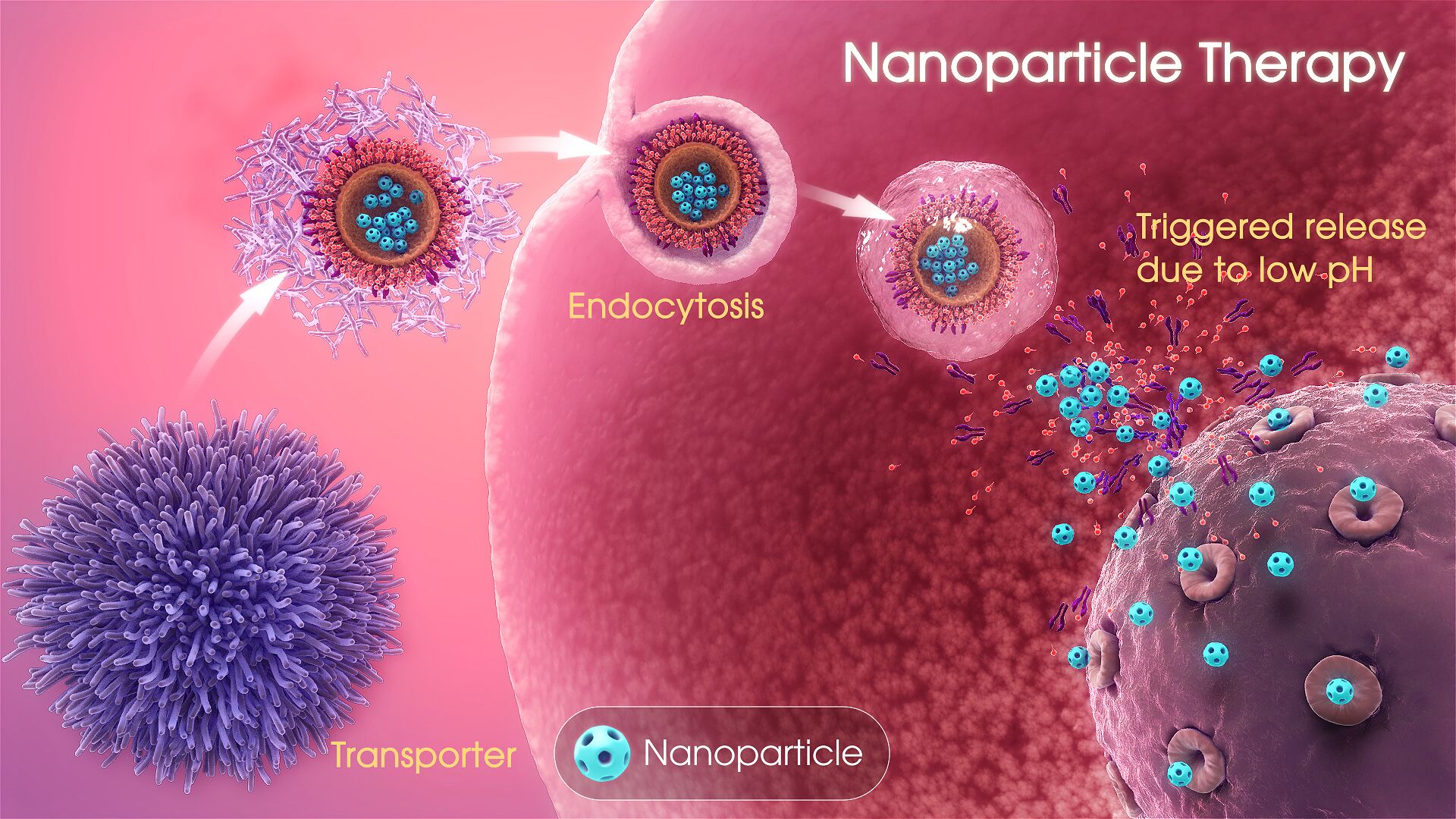
Targeting nanoparticles (either passively or actively) enhances the intracellular concentration of therapeutic drugs in cancer cells while avoiding toxicity in normal cells. In addition, the targeted nanoparticles can also be designed as either pH-sensitive or temperature-sensitive carriers. The pH-sensitive drug delivery system can deliver and release drugs within the more acidic microenvironment of the cancer cells and/or components within cancer cells.
However, there is a challenge that nanoparticles might change the stability, solubility, and pharmacokinetic properties of the carried drugs. The shelf life, aggregation, leakage, and toxicity of materials used to make nanoparticles are other limitations for their use. Materials like poly-lactic-co-glycolic acid (PLGA) have low toxicity, but degrade quickly and do not circulate in tissues long enough for sustained drug delivery. On the other hand, materials such as carbon nanotubes and quantum dots are durable and can persist in the body for weeks, months, or even years, making them potentially toxic and limiting their use for repeated treatments. New materials to make targeted nanoparticles such as silicon/silica (solid, porous, and hollow silicon nanoparticles) have been developed; however, their use for drug delivery to cancer patients has taken off slowly due to the potential health risks associated with introducing new materials in the human body.
So far, scientists have experimented with drug-filled nanoparticles in the treatment of various types of cancer, including breast cancer and endometrial cancer.
4. Starving Tumors
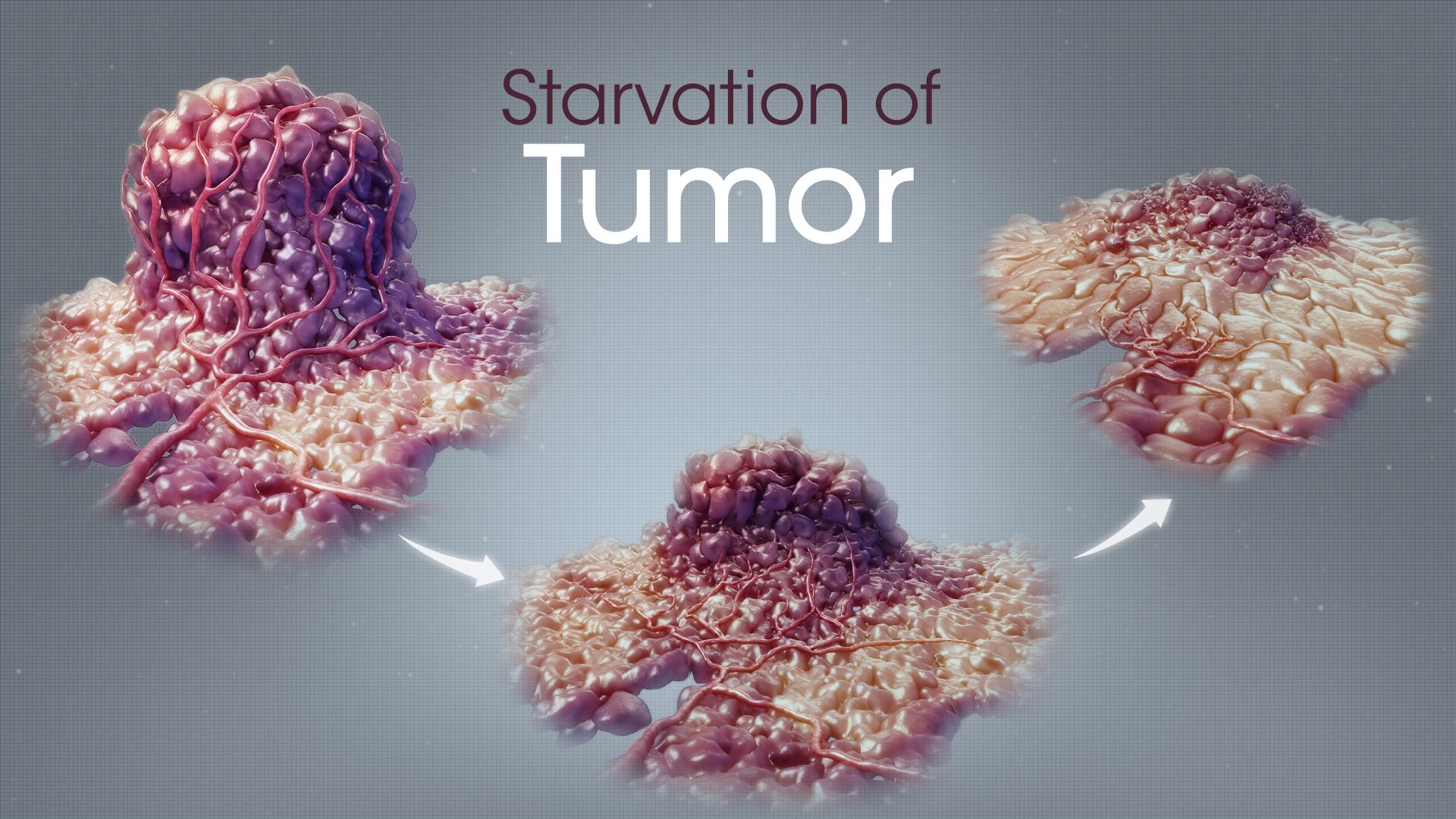
This involves stopping glutamine from feeding and supporting the growth of cancer cells, especially breast, lung and colon cancers. Glutamine deficiency maximizes the impact of oxidative stress, eventually leading to cell death. Another way to starve tumors is by blocking access to Vitamin B2. This strategy could help individuals avoid the toxic side effects of chemotherapy.
5. Personalized Medicine
Up till now, people with a certain type and stage of cancer received the same treatment. But now, doctors understand that the solution that helps one person may not work well for someone else.
Our genes can now give doctors a better idea which treatments will help us the most.
Targeted drugs too, instead of wiping out all cells (including healthy ones), can focus just on deadly cancer cells. For instance, a drug called PEGPH20 has been tested to treat even stage IV pancreatic cancer if their cancer cells have a high level of hyaluronic acid sugar.
This is still an evolving approach and despite the promises of personalized cancer treatments, not all types of cancer have personalized treatment options. Some personalized treatments are only offered through a clinical trial and are not yet standard treatment options. Genetic testing for patients and tumor samples may be costly and time-consuming. Besides, doctors still don’t know all about the genetic changes that occur in a cancer cell. They also don’t know how some of these new cancer treatments work. A targeted therapy may stop working, making a promising treatment no longer effective.
Conclusion
While the emerging research in oncology is bringing in more and more effective ways of controlling cancer, most of them are still nascent and have been only confined to experiments. The above treatments offer hope that medicine is moving towards a time when both the tools and the knowledge about cancer will grow to the point that most forms of cancer will be considered to be very treatable.








